Fungal acne causes and treatments

Fungal Acne: Causes, Symptoms, and Effective Treatments
Fungal acne, also known as Pityrosporum folliculitis or Malassezia folliculitis, mimics the appearance of hormonal or bacterial acne but is a distinct condition caused by an overgrowth of yeast rather than bacteria. Here’s everything you need to know about this condition, from its causes to its treatments.
What is Fungal Acne?
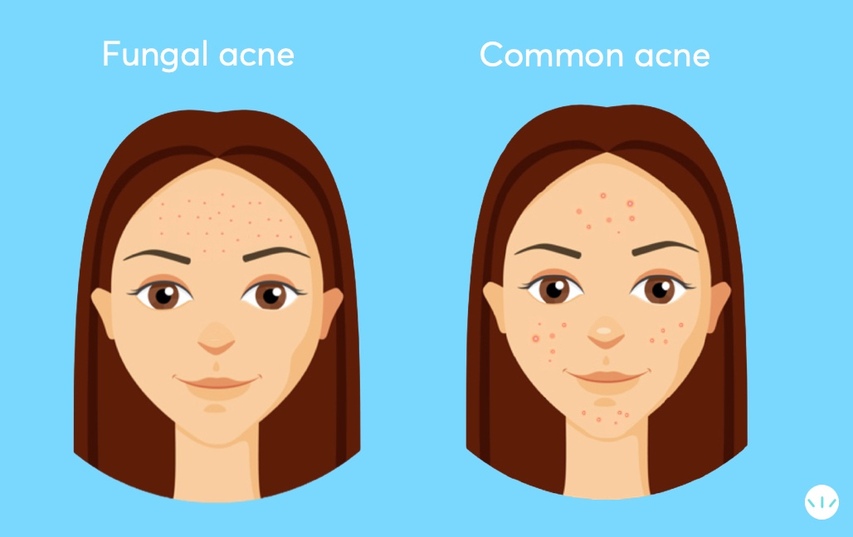
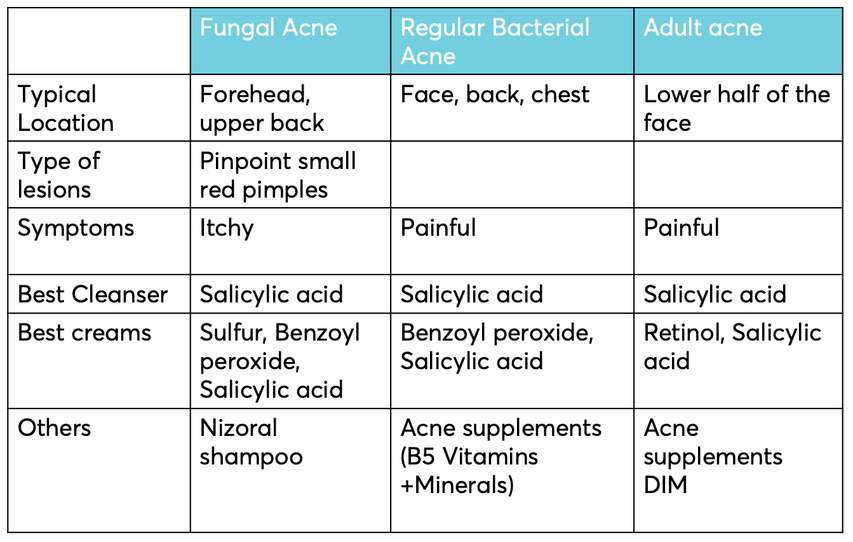
Fungal acne is a skin infection caused by the overgrowth of yeast (Malassezia), a natural part of the skin’s microbiome. Unlike bacterial acne, which often includes a variety of lesion types (blackheads, whiteheads, and cysts), fungal acne typically appears as small, uniform red bumps or pustules that are often itchy. These bumps occur when the yeast feeds on excess oil from the skin’s natural sebum or oil-based skincare products.
In some cases, this condition leads to Tinea versicolor, while in others, it manifests as an infection of the hair follicles resembling traditional acne.

Where Does Fungal Acne Appear?
Fungal acne thrives in oil-rich areas of the skin, including:
- Face: Forehead, sides of the nose, and chin (T-zone).
- Body: Upper back, chest, and shoulders.
These areas overlap with where bacterial acne and seborrheic dermatitis often appear. If you’re unsure of the exact condition, consult a dermatologist for a diagnosis.
Causes of Fungal Acne
Fungal acne can develop when the balance of the skin's microbiome is disrupted. Common triggers include:
- Climate: Warm, humid environments encourage yeast growth. Studies show higher rates of fungal acne in tropical climates.
- Antibiotics: Prolonged use of antibiotics, such as clindamycin or doxycycline, can kill bacteria on the skin, allowing yeast to overgrow.
- Hygiene and Sweat: Wearing sweaty clothes for extended periods or not properly cleansing after workouts can create the ideal environment for yeast.
- Oil-based Skincare Products: Yeast feeds on oils, so using oil-rich creams or makeup can trigger fungal acne.
- Diet: High sugar intake can exacerbate fungal acne, as yeast thrives on sugar.
- Steroids: Oral or topical corticosteroids, as well as bodybuilding hormones, can disrupt the skin's microbiome and trigger fungal acne.
- Face Masks: Prolonged use of face masks traps heat and humidity, creating a breeding ground for yeast.

How to Identify Fungal Acne vs. Bacterial Acne
Fungal acne typically appears as small, identical, itchy red bumps, while bacterial acne may consist of various lesion types, including blackheads, whiteheads, and cysts. If your acne is unresponsive to traditional treatments, it may be fungal acne.
Best Treatments for Fungal Acne
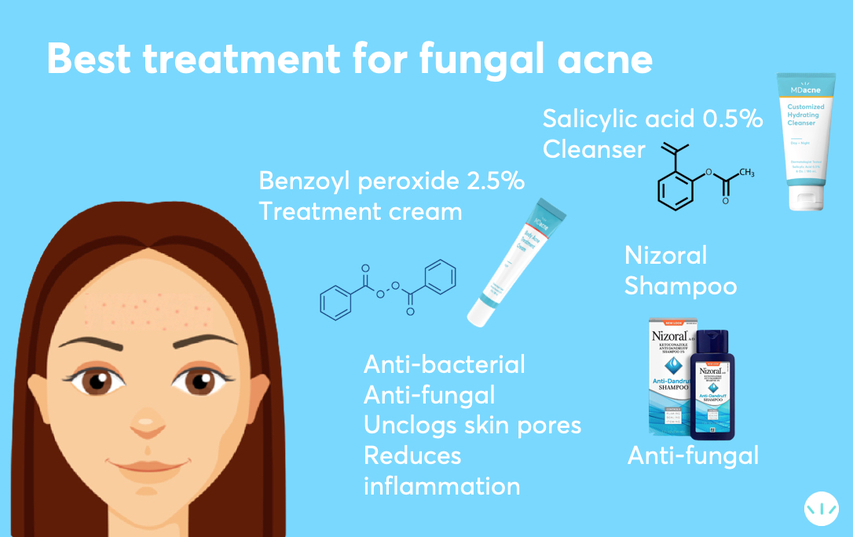
1. Anti-Fungal Shampoos and Cleansers
- Ketoconazole Shampoo (e.g., Nizoral): This is one of the most effective treatments for fungal acne. Use as a body wash every other day, leaving it on the skin for 3–5 minutes before rinsing.
- Salicylic Acid Cleansers: These exfoliate dead skin cells, unclog pores, and enhance the effect of anti-fungal shampoos.
2. Medicated Creams
- Ketoconazole 2% Cream: Available by prescription, this cream targets fungal infections directly.
- Benzoyl Peroxide: A strong antimicrobial agent that combats both bacteria and yeast.
3. Body-Specific Treatments
- For body fungal acne, use stronger products like benzoyl peroxide 5% combined with tea tree oil. These ingredients target fungi and reduce inflammation.
4. Moisturizers
- Use an oil-free moisturizer to prevent further feeding the yeast. Opt for products designed for acne-prone skin.
5. Hygiene Practices
- Change out of sweaty clothes promptly and cleanse your skin thoroughly after workouts. Use breathable fabrics and avoid re-wearing unwashed clothing.
6. Diet Adjustments
- Reduce sugar and simple carbohydrate intake to minimize yeast overgrowth.
How to Use Nizoral for Fungal Acne
Apply Nizoral shampoo to affected areas daily or every other day for three weeks. Massage into the skin, leave it for 3–5 minutes, then rinse. Once fungal acne clears, continue using it twice weekly for maintenance.
Preventing Fungal Acne
- Choose the Right Skincare Products: Avoid oil-based products and look for non-comedogenic options.
- Use Anti-Fungal Face Masks: If wearing a mask is necessary, opt for cotton masks infused with anti-fungal agents like copper or silver ions.
- Avoid Prolonged Antibiotics: Consider alternative treatments for acne to prevent disruption of the skin’s microbiome.
Frequently Asked Questions
Q: Can fungal acne last long?
A: Untreated fungal acne can persist for weeks or months. With the right treatments, it often improves significantly within a few weeks.
Q: Can COVID masks cause fungal acne?
A: Yes, the heat and humidity trapped under masks create an ideal environment for yeast. Opt for breathable, anti-fungal masks to prevent breakouts.
Q: Does tea tree oil help with fungal acne?
A: Yes, tea tree oil has strong anti-fungal properties, especially when combined with salicylic acid or benzoyl peroxide to penetrate clogged pores.
Conclusion
Fungal acne can be stubborn, but with the right approach—including anti-fungal shampoos, targeted skincare products, and healthy lifestyle practices—it can be effectively managed and prevented. If you’re unsure about your condition or need personalized advice, consult a dermatologist to determine the best treatment plan for your needs.
Shop:
Best Acne treatment cream with Salicylic acid 2% (BHA)
Best Acne treatment cream with Benzoyl Peroxide 2.5%
Best Acne treatment cream with Benzoyl Peroxide 5%
References:
Malassezia (Pityrosporum) Folliculitis
Pityrosporum folliculitis: diagnosis and management in six female adolescents with acne vulgaris
Steroid acne vs. Pityrosporum folliculitis: the incidence of Pityrosporum ovale and the effect of anti-fungal drugs in steroid acne
Differential diagnosis of facial acne on black skin.
Microorganisms inhabiting follicular contents of facial acne are not only Propionibacterium but also Malassezia spp.
To find the right acne treatments for your unique skin, take the free skin assessment by clicking here.